

There are 500,000 new cancer cases in Germany alone every year. Experts expect this figure to increase by almost 20 percent by 2030. Currently, the most common cancers in men are prostate, lung, and bowel cancer, while in women they are breast, bowel, and lung cancer. Besides the well-known treatment options such as surgery, chemotherapy, and radiotherapy, there are now also highly advanced new methods. One of the innovative approaches is so-called CAR T cell therapy, which is used at Helios Hospital Berlin-Buch, among other places.
(Published: February 2024)
Fresenius editor Brigitte Baas spoke to Prof. Bertram Glaß, Chief Physician for Hematology and Cell Therapy at Helios Hospital Berlin-Buch, about the opportunities and risks associated with this treatment.
Professor Glaß, please briefly explain the principle of CAR T cell therapy and how this form of therapy works.
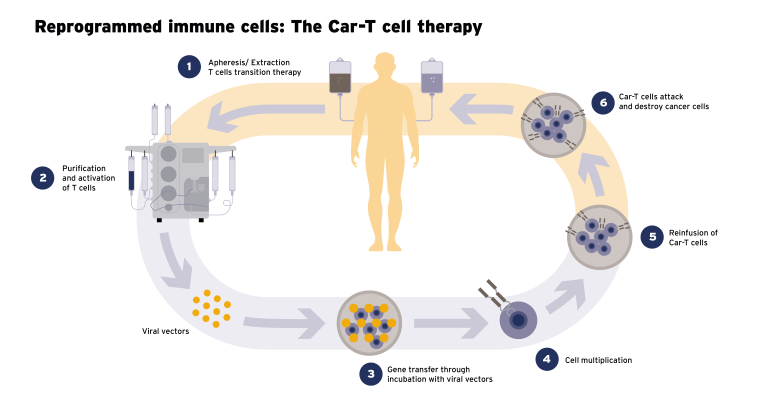
Prof. Bertram Glaß: CAR T cell therapy is a form of immunotherapy that uses the patient’s defense cells to target and destroy malignant cells and – unlike standard chemotherapy, for instance – leave healthy tissues and organs largely intact. We firstly remove the patient’s own T cells, which play a key role in the body’s immune system, and genetically modify them. These T cells subsequently acquire the ability to recognize cancer cells. The cells are then given back to the patient via a drip – with the aim of initiating processes within the body to destroy the cancer cells. To date, this type of therapy has been available for the treatment of specific tumors of the human immune system. Extending the therapy to treat other common tumors is the subject of ongoing scientific investigations. (Read more about this in the box)
In other words, each form of CAR T therapy is produced for a specific person with a specific medical condition. Is this the personalization that is being talked about a great deal at the moment? And what exactly are the advantages of such a form of treatment from the patient’s perspective?
Prof. Glaß: CAR T therapy is certainly a first step and a potential basis for truly personalized medicine in the future. At the same time, there are other approaches – such as other forms of immunotherapy or the identification of cancer-specific genetic changes in the cancer cell – which are covered by special drugs. All these approaches are combined in personalized tumor medicine, permitting highly targeted treatment of the precise disease affecting a specific patient. Compared to a one-size-fits-all approach, this can be more effective at fighting tumors, while at the same time producing effective therapies with fewer side effects. Furthermore, personalization makes it possible to adapt treatment over the course of the disease, making it generally more precise and efficient than anything we’ve had in the field of cancer medicine to date.
For which types of cancer does CAR T cell therapy represent a promising approach?
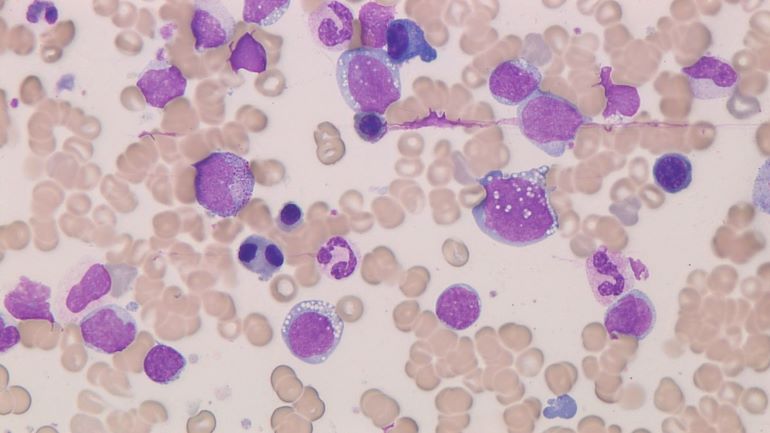
Prof. Glaß: At present, CAR T cell therapy has been approved to treat two groups of diseases in Germany and other European countries. It can currently be used for certain malignant diseases of the immune system and hematopoiesis – such as acute lymphocytic leukemia (ALL) and some types of non-Hodgkin’s lymphoma (NHL) and multiple myeloma. These are considered hard to treat, particularly in the event of a relapse after initial forms of therapy. For these cancers, there is an overall response rate of up to 80 percent with CAR T cell therapy, with long-lasting remission – i.e., possible cures – in 40 to 50 percent of cases. This means that four fifths of all patients can be helped with treatment!
As with any kind of therapy, there are bound to be side effects with CAR T cell therapy. What are they?
Prof. Glaß: In addition to cancer cells, the CAR T cell process also has an effect on healthy immune cells. The process is highly effective and can cause side effects due to the severe inflammatory response and possibly also due to the effect it has on certain unconnected healthy cells within the nervous system. Various symptoms may therefore occur following the CAR T cell infusion therapy, including fever, shivers, low oxygen levels in the blood, rapid heartbeat, and low blood pressure. Disorders of the nervous system are also possible, along with infections and a lack of antibodies. The good news is that we keep a close eye on all these potential side effects. We can treat all of them well and they will pass. Overall, the relationship between effect and side effect is considerably more favorable than is the case with older methods such as high-dose chemotherapy, which is why they are increasingly being replaced by CAR T therapy.
CAR T therapy is certainly a first step and a potential basis for truly personalized medicine in the future.
World Cancer Day is on February 4. The theme of the campaign is “Close the Care Gap.” This gap in care relates to the access that cancer patients have to diagnosis and treatment. How can CAR T cell therapy help to close this gap?
Prof. Glaß: Admittedly, access to cancer care varies considerably around the world. Here in Germany, it has to be said that we are in a very good position in terms of diagnosis and therapy. As far as therapy is concerned, there are always gaps in care in our country wherever our scientific knowledge is not yet sufficient to establish an effective – and, if possible, curative – form of therapy. In the case of leukemia, lymphoma, and multiple myeloma, it has now been possible to reduce this gap. Yet CAR T cell therapy also offers real hope when it comes to closing the gaps for other types of cancer that cannot yet be cured with treatment. Currently, however, only a very small number of patients can benefit from this innovative form of treatment – and only in developed countries such as ours. That’s because it is very complex and therefore expensive, and it has so far only been used in instances where other therapy options have failed.

What exactly is the reason for this? And how could CAR T cell therapy be made available to more patients and to treat other types of cancer?
Prof. Glaß: This form of therapy is expensive and complex because the production process for the CAR T cells takes a very long time and must be undertaken individually for each patient. It is currently around 14-28 days. We are dealing with living cells here, which are worked on in highly complex factories under the strictest controlled conditions. The supply chain is also highly complex and needs certain structures. For instance, the hospital must have its own highly skilled hematology center. Not even all maximum care hospitals meet these requirements. However, considerable efforts are now being made within the sector to shorten the production process and make it cheaper.
So far, we have talked a great deal about how cancer can be treated, but Helios is also currently highlighting the importance of cancer prevention and early detection. What importance do you as a practitioner attach to prophylaxis?
Prof. Glaß: We all know that the earlier cancer is detected, the easier it generally is to treat, the better the success rate, and the higher the chances of survival. In this particular context, early cancer detection represents perhaps the greatest potential for therapy! Doctor’s check-ups with blood and urine tests are one important aspect, along with mammography, colonoscopy, and skin cancer screening. The aim is always to detect cancer and its precursors as early as possible.
What else is important in terms of prophylaxis?
Prof. Glaß: If it is to be effective, we must also mention primary prevention. The aim here is to prevent cancer from developing in the first place. This includes measures such as eating a healthy, balanced diet, avoiding alcohol and nicotine, protecting the skin from UV light, and much more besides. Ultimately, primary prevention covers the aspects that each and every one of us can influence the most. The astonishing thing about this is that primary prevention and early detection together could reduce cancer mortality by up to 75 percent.
Yet, time and again, experts find that many people do not take advantage of this potential at all. Why do you think this is?
Prof. Glaß: Well, that is most likely due to human psychology. As long as there is no damage, the risk is too abstract. And there are always examples of people for whom everything has gone well – chain-smokers who live to be 90 years old. These rare examples are then cited as proof when people drink a lot, eat too much sugar and fat, and do not exercise enough. For many, a certain sense of fatalism undoubtedly plays a role: Since certain types of cancer develop largely by chance – such as lymphomas, brain tumors, and childhood cancers – they can hardly be prevented by embracing a healthy lifestyle on the basis of current knowledge. But treating a patient here in the hospital and literally saving their their life – and then seeing them smoking outside by the door, that is clearly the really hard part of our job. Yet even that doesn’t stop me from hoping that one day we will find effective forms of therapy for all types of cancer. There is so much innovation happening right now – and we are a part of it!
ⓘ CAR T cell therapy
In CAR T cell therapy, the body’s T cells, which are part of its defense or immune system, are enriched with so-called CARs. CAR stands for chimeric antigen receptor. The removed T cells are genetically modified in the laboratory. As a result of this genetic change, the T cells acquire the ability to recognize cancer cells that carry a specific target antigen on their surface. This target antigen is often characteristic of certain types of cancer. The T cells have thus become CAR T cells.
These are then fed back into the patient’s body via a drip and they circulate in the bloodstream. When they encounter cancer cells with the specific target antigen, the extracellular domain of the CAR specifically binds to this antigen on the surface of the cancer cell and activates the CAR T cell. This leads to a rapid proliferation of T cells and the release of cytotoxic molecules that destroy the cancer cell.
One key aspect of CAR T cell therapy is the ability of the modified T cells to maintain a long-term immune response in the patient’s body. This can help to sustain repeated attacks on cancer cells over a longer period of time. The exact way in which it works may vary depending on the specific protocols and target antigens used in the therapy.
Contact
Helios Klinikum Berlin-Buch
Schwanebecker Chaussee 50
13125 Berlin
T +49 (0)30 94 01-0

